What Happens During Cataract Surgery?
During the surgery, the natural lens (now a cataract) is removed, and an artificial lens in implanted. Two small incisions are made, constructed in such as way that nearly all will seal without sutures (stitches). The shell that holds the cataract in place (the capsule) is opened.
Phacoemulsification (a technique involving a small ultrasonic probe) is then used to remove the cataract from the capsule. This surgical technique allows the cataract to be removed through very small incisions (instead of removing it as a whole).
That said, rare cases are not amenable to this technique. The artificial lens (intraocular lens or IOL) is then inserted through the small incision into the capsule, which holds it securely in place. While cataract surgery can greatly reduce a patient’s dependence on glasses, there is still a chance of needing glasses for the clearest vision possible post-operatively.
Each patient is unique, and the surgeon reviews this for every individual. Additional options are available for most patients who are seeking to further reduce their glasses dependence after surgery.
Cataract Evaluation
If you are coming in to the office for a cataract evaluation, there are several steps to expect. First, a technician will take a detailed history of all medical conditions, medications, and prior procedures. Please bring a list to ensure an accurate record. Your pupils will likely be dilated during this visit. This allows for a detailed examination of the cataracts are other structures of the eye. It also means that your vision will be blurry for several hours. It is mostly near vision that is affected by these drops, but please plan to bring someone with you in case you are unable to return home safely alone. You will have a thorough examination by one of our surgeons.
If cataract surgery is being considered, you will have measurements of the eyes. These measurements provide the information necessary to chose the appropriate IOL (artificial lens) power and surgical plan for you specifically. At this point, your surgeon will discuss the options available to you, including whether you are a candidate for the premium IOLs and laser-assistance. You will have a comprehensive discussion with your surgeon about the surgery. Finally, you will meet with the surgical coordinator to set a specific date for the procedure and to review the logistical details of surgery. A cataract evaluation, with all steps above, takes longer than a comprehensive eye exam. Please allow for up to two hours for this entire process.
Are You a Candidate for Cataract Surgery?
Take Our Self-Test!
IOL Options

Standard IOL
A standard monofocal IOL corrects for a single distance. Most patients chose to set the eye either for far distance or near work. A discussion with the surgeon can help guide a patient to the best decision for that individual.
Some patients with cataracts in both eyes chose the option of monovision. This is when one eye is set for far distance while the other is set for near, reducing the dependence on glasses significantly. Not everyone is tolerant of monovision. This involves a thorough discussion prior to surgery.
Mini monovision is a compromise between mono vision (described above) and single distance vision. With mini monovision, one eye is set for far distance and the other eye is set for an intermediate distance (approximately an arm’s reach). This reduces glasses dependence for many things, but reading glasses are still required to do near work. Because the difference between the two eyes is small, it is more widely tolerated by patients than full monovision.

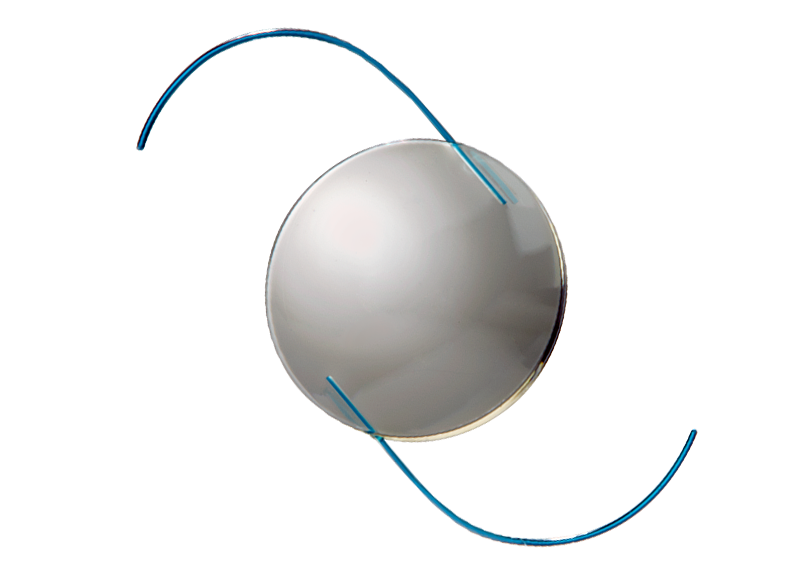
Toric IOL
Toric IOLs are premium lenses that reduce corneal astigmatism. Corneal astigmatism occurs when the curvature of the cornea is irregular. Many doctors use the analogy of a football shaped cornea (one with astigmatism) versus a basketball shaped cornea (one without astigmatism) to help illustrate this concept. A Toric IOL has the power required to reduce this astigmatism built into the lens, allowing for greater glasses independence. The effect of uncorrected astigmatism on vision is blurring or distortion. If astigmatism is present, and not reduced during surgery, the astigmatism can still be corrected in glasses or contact lenses.
Toric IOLs come in monofocal, extended depth, and multifocal lens variations. The monofocal version gives a single focal distance as described above, but with astigmatism reduction. The other versions are described below.
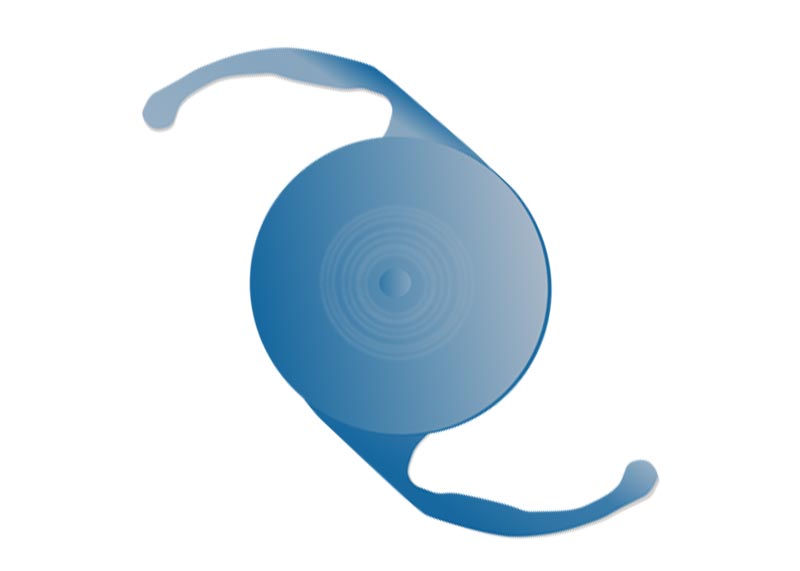
Multifocal IOL
Multifocal IOLs are premium lenses which allow for both far distance and near vision in a single lens. These lenses can very successfully minimize glasses dependence. Unfortunately, not all patients are candidates for this type of lens. There are some optical compromises to these lenses to get the range out of glasses, which will be thoroughly discussed for all patients considering this lens. A detailed examination and discussion with the surgeon is necessary to determine which patients are candidates.

Extended Depth of Focus IOL
Extended Depth of Focus IOLs are the newer generation of the multifocal IOLs. These premium lenses allow for far distance through intermediate zone vision in a single lens. Typically, this ranges from things far away through approximately computer and tablet distance and includes larger print near work, without glasses. The side effect profile is quite minimal with this type of lens and it may be offered to more patients than the multifocal lenses. This lens will give a greater degree of glasses independence than the standard, but patients should expect to still wear a low power pair of reading glasses for very small print. Again, a detailed examination and discussion with the surgeon is necessary to determine which patients are candidates.
Accommodating IOL
Accommodating IOLs are premium lenses which allow an increased range of vision at different distances. This lens can decrease the need for glasses. It is similar in goal to the multifocal lenses listed above; however, this lens works by a different mechanism and often has a slightly more limited range of glasses independence. It also has a different possible side effect profile.
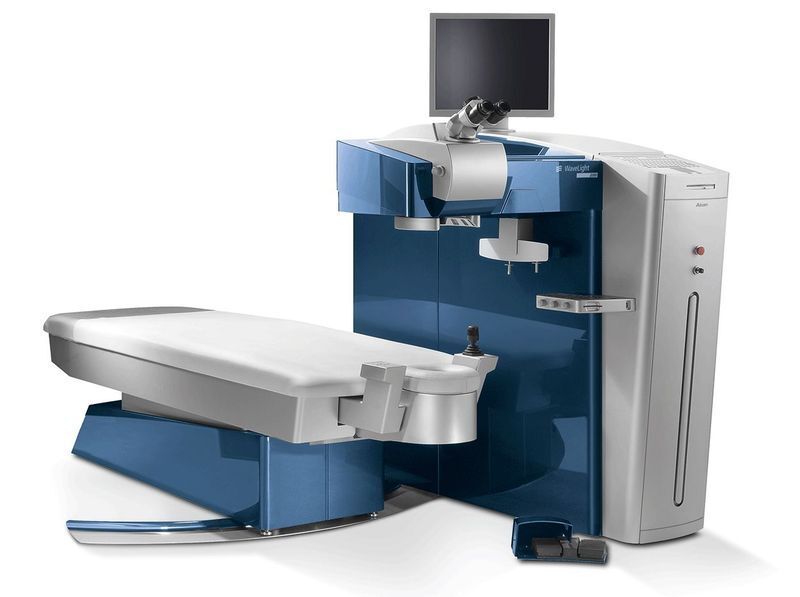
Laser-assisted Cataract Surgery
The femtosecond laser is cutting edge technology used to assist in cataract surgery. The laser does several stages of the cataract surgery, including the critical steps of opening the capsule (the shell surrounding the cataract) and softening the cataract. It also reduces mild to moderate levels of astigmatism. Laser-assistance can minimize the amount of ultrasound energy required to remove the cataract, allowing for less swelling and a faster recovery. It can improve the safety of surgery in certain patients. The laser can also aid in the precision of intraocular lens (IOL) placement. Precise IOL positioning is crucial, especially for some patients choosing the premium IOLs listed above.
Intraoperative Wavefront Aberrometry
Intraoperative wavefront aberrometry is newly available technology which allows the surgeon to verify or refine the power of the IOL during surgery. This is helping to further minimize the need for glasses after surgery in many patients. It is especially useful in patients who have had prior refractive surgery including LASIK.
Risks of Cataract Surgery
While cataract surgery is extremely successful, there are, of course, risks with any surgery. The surgeon will review risks specific to each patient prior to surgery. All questions about risk will be addressed in the office. A common question involves whether the cataract will ever “grow back.” Cataracts do not recur after surgery. Some patients may develop a clouding of the capsule (the shell holding the artificial lens) in the months or years after surgery. This is called a posterior capsule opacification. This condition is treated easily with a laser procedure called a laser capsulotomy. The procedure takes only minutes and is painless.

